The federal government seeks authority over stem cell treatments but risks thwarting medical advancement.
Two years ago, the U.S. Food and Drug Administration (FDA) filed a lawsuit in a federal district court in California that could determine the reach of its regulatory authority over how people use their own stem cells.
The FDA stem cell lawsuit has potentially precedent-setting implications for the future of stem cell and regenerative medical research, medical technology advancement in clinical applications, the expansion of patient health care options, and the control of the rise of private and public health care expenditures.
The repercussions of using human stem cells in medical research and practice could be the most seismic since Henrietta Lacks and her versatile HeLa cells. Lacks’s “immortal” HeLa cells have been used to study the effects of toxins, drugs, hormones, and viruses on the growth of cancer cells. They have also played a critical role in the development of the polio vaccine and in vitro fertilization treatments.
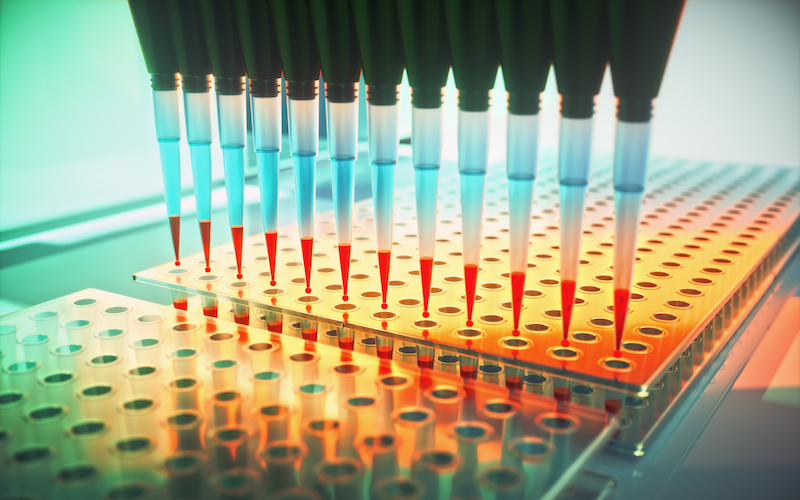
The “primordial” stem cells in stromal vascular fraction (SVF)—cellular extract produced in a laboratory from fat—may hold similar promise in researching and treating a broad range of medical conditions, such as orthopedic problems, cardiovascular diseases, and autoimmune disorders.
The defendants sued by FDA in its recent litigation—California Stem Cell Treatment Center, Inc. and its founders, physicians Elliot Lander and Mark Berman—argue that FDA has no regulatory authority over their SVF stem cell procedures, which the defendants claim have helped countless patients heal from serious ailments, such as arthritis, chronic pain, and other inflammatory conditions. Their procedures are autologous—extracted from one person and administered to the same person. In an interview, Berman details his grievances with FDA and what he deems is an illegal assertion of regulatory power over autologous stem cell therapy and SVF in particular.
In its lawsuit, FDA argues that Lander and Berman’s use of SVF violates the Food, Drug, and Cosmetic Act (FDCA) because it qualifies as a “drug,” which must be subjected to the FDA clinical trial process before market approval. FDA recently doubled-down on this position in response to a call from researchers and practitioners for a reevaluation of its regulation of SVF and other fat-derived stem cell products. A federal district court judge in Florida recently upheld this position in an FDA lawsuit against SVF provider U.S. Stem Cell Clinic, LLC.
In Lander and Berman’s SVF process, adipose—or fat—is extracted from the patient. Collagenase enzymes and a centrifuge are then used to separate the SVF from the fat. The resulting product is then administered to the same patient. The defendants argue that their SVF process falls under the “same surgical procedure” exception to the FDCA and is thus outside the scope of FDA regulatory power. Unlike the defendants in United States v. U.S. Stem Cell Clinic, LLC, Lander and Berman recently defeated FDA’s motion for summary judgment, which means the issue will go to trial.
Although the central issue in the case is one of technical statutory interpretation, the result could be seismic in the fields of regenerative and cellular medicine.
A victory for Lander and Berman could have broad implications for immediate patient access to stem cell therapy and could mark the beginning of a potential further loosening of FDA stem cell restrictions.
Any SVF procedure that returns a patient’s own stem cells during a “point of care” surgical procedure would be off limits to FDA, and regulatory authority would likely devolve to the state level. State medical boards, medical malpractice and consumer protection laws, voluntary patient databases, and physician credentialing agencies could then coordinate to ensure professional and patient safety standards are met.
The implications for medical research are also significant. If SVF is not restricted under the FDCA, this could facilitate data collection in the clinical setting, effectuating the standardization of SVF processing methods and the development of best practice standards in an industry that is likely to expand. This could reduce inherent surgical risks, such as sample mishandling and contamination.
Standard practice methods could also help optimize cellular yield, make post-delivery cellular survival possible, and establish recommended dose guidelines for specific medical conditions.
A court victory for Lander and Berman could also lead to more methodologically rigorous studies being published in academic journals, making the industry as a whole more robust.
The current SVF litigation also has important implications for patients. With the number of Americans with chronic illnesses rising, medical technology must evolve to meet their needs. According to the Centers for Disease Control and Prevention, six in ten adult Americans have a chronic illness and four in ten have two or more such illnesses.
Furthermore, the Partnership to Fight Chronic Disease reports that chronic disease is the leading cause of death and disability in the United States, responsible for seven out of every ten deaths. Chronic diseases account for 81 percent of hospital admissions, 91 percent of all prescriptions filled, and 76 percent of all physician visits. In 2005, for example, 75 percent of all private and public health care expenditures went toward treating chronic illness. Many of these conditions involve chronic inflammation, which SVF has been shown to treat successfully.
As FDA attempts to increase its regulatory enforcement authority over clinics offering stem cell products, it may simultaneously be on the verge of a significant loss for patients if it should win.